views

[176 Pages Report] Fraud analytics is the efficient use of data analytics and related business insights developed through statistical, quantitative, predictive, comparative, cognitive, and other emerging applied analytical models for detecting and preventing healthcare fraud.
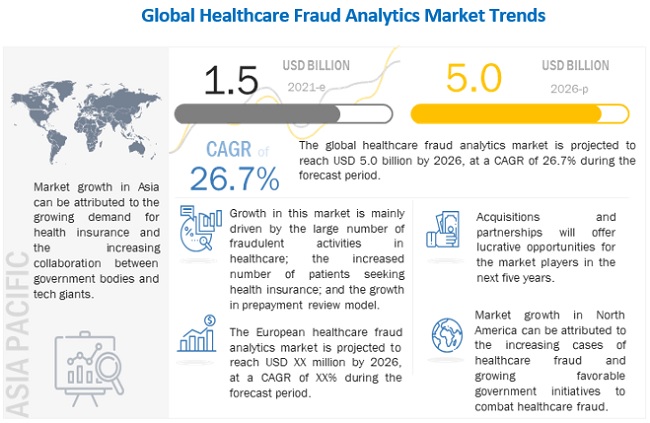
The global healthcare fraud analytics market is projected to reach USD 5.0 billion by 2026, at a CAGR of 26.7% during the forecast period. Market growth can be attributed to a large number of fraudulent activities in healthcare, increasing number of patients seeking health insurance, high returns on investment, and the rising number of pharmacy claims-related frauds. However, the dearth of skilled personnel is expected to restrain the growth of this market.
The global market is facing a plethora of challenges. Travel bans and quarantines, halt of indoor/outdoor activities, temporary shutdown of business operations, supply demand fluctuations, stock market volatility, falling business assurance, and many uncertainties are somehow exerting a partial negative impact on the business dynamics.
Many healthcare providers and specialists have been observed to be engaged in fraudulent activities, for the sake of profit. In the healthcare sector, fraudulent activities done by patients include the fraudulent procurement of sickness certificates, prescription fraud, and evasion of medical charges.
For More Info, Download PDF Brochure @ https://www.marketsandmarkets.com/pdfdownloadNew.asp?id=221837663
Over the years, the number of people benefitting from various healthcare schemes has grown considerably. A couple of reasons contributing to the growth of the health insurance market include the rise in the aging population, growth in healthcare expenditure, and increased burden of diseases. In the US, the number of citizens without health insurance has significantly decreased, from 48 million in 2010 to 28.6 million in 2016. In 2017, 12.2 million people signed up for or renewed their health insurance during the 2017 open enrollment period (Source: National Center for Health Statistics).
Emerging markets such as Asia promise significant growth in health insurance coverage, mainly due to increasing government initiatives, rising government and private investments for promoting medical insurance, and growing income levels. This growth is aided by the increasing affordability of health insurance for the middle class in this region and the rising awareness regarding the benefits of health insurance.
In the UAE, as per a new regulatory policy (2017), any citizen residing and working in the UAE needs to be insured medically. Such regulatory changes in the buying behavior of employers (from employer-based plans to providing individual spending allowances to the staff) are driving the health insurance market in the region.
As per the US Department of Health and Human Services findings of 2018, national Medicaid data has shortcomings that could hinder the process of fraud detection in the public sector. The OIG claims that Medicaid data is often incomplete and inaccurate; this affects the process of detecting fraudulent claims and results in the wastage of billions of dollars due to FWA.
The prominent players in Healthcare Fraud Analytics Market are IBM Corporation (US), Optum, Inc. (US), Cotiviti, Inc. (US), Change Healthcare (US), Fair Isaac Corporation (US), SAS Institute Inc. (US), EXLService Holdings, Inc. (US), Wipro Limited (India), Conduent, Incorporated (US), CGI Inc. (Canada), HCL Technologies Limited (India), Qlarant, Inc. (US), DXC Technology (US), Northrop Grumman Corporation (US), LexisNexis (US), Healthcare Fraud Shield (US), Sharecare, Inc. (US), FraudLens, Inc. (US), HMS Holding Corp. (US), Codoxo (US), H20.ai (US), Pondera Solutions, Inc. (US), FRISS (The Netherlands), Multiplan (US), FraudScope (US), and OSP Labs (US).












